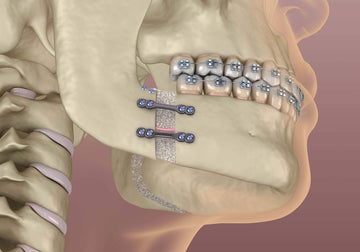
Maxillofacial deformities, congenital, developmental or acquired, may manifest during growth or at adult life functional, cosmetic or psychological problems.
The treatment of such malformations, affecting one or multiple bones of the facial skeleton, involve multidisciplinary team of orthodontist, maxillofacial surgeon, pediatric dentist, head and neck surgeon, speech therapist, psychologist, etc.
This skeletal alteration is first diagnosed during childhood and is accentuated throughout the period of cranio-facial growth .
The disharmony caused by the fact that one part of the skeleton suffers an excess of growth or deficit while the rest have a normal development, will be accompanied by an occlusal alteration. This is the reason why the orthodontist, in most of the cases, is the first to diagnose the deformity.
He will review the medical history, patient concern (functional or esthetic), if it is a congenital or developmental problem, stable or progressive, etc.
Blair concluded: “Treating of skeletal deformities is really surgical work, but the earlier a competent, congenial orthodontist is associated with the case, the better it will be for both the surgeon and the patient.”(1)
Although the field of orthognathic surgery has changed tremendously since the early 1900s, the role of an orthodontist in achieving an ideal and stable result remains pivotal.
Initial evaluation to diagnose the deformity include intra-oral orthodontic photographs, articulated study models, TMJ position, panoramic radiography, a lateral and a postero-anterior cephalogram, three-dimensional (3D) photographic images,(2) 3D cone beam radiographs,(3) video images of the patient.(4)
Posterior Transverse Dimension
This must be analyzed with teeth or models in the proposed post-surgical position. In a patient with a class II skeletal malocclusion the patient will posture their mandible forward into a position with a proper over-jet. In a patient with a class III skeletal malocclusion, orthodontic models are placed in the proposed post-surgical position. The second step is to identify if the cause is at the upper or lower jaw, if it is skeletal or dental. The mandible is rarely found to have transversal discrepancies, that is why is considered the diagnostic arch and its skeletal dimension is rarely questioned.
The the position of the cusps predict transversal deficiency: the lingual cusps of the mandibular molars should be at or slightly below the level of the buccal cusps. If the lingual cusps are significantly below the buccal cusps, this represents constricted mandibular molars. In the maxilla, the buccal cusps of the molars should be at or slightly above the lingual cusps. If the buccal cusps are below the lingual cusps, this represents constricted maxillary molars.
Model surgery must be performed to place the molars in their correct position if the transverse deficiency is severe. If the discrepancy is minor, the re-positioning of the molars can be estimated on the study models.
In orthognathic patient, maxillary transverse discrepancy can be eliminated through surgically assisted rapid palatal expansion (SARPE), orthodontic dental compensation, or segmentation of maxilla.
Vertical and Sagittal Skeletal Relationship
When analyzing an orthognathic patient, it is critical to appreciate the relationship between the vertical and the sagittal dimension and it is usually appreciated on cephalometric analysis. The clockwise or anti-clockwise rotation of the mandible ,the Wits appraisal, mandibular angle and several well known analyses can contribute to the diagnosis.
Cephalometric X-rays have been the standard image taken as part of orthodontic work up and is used for : diagnosis, monitoring the jaw growth and occlusal change prior to orthognathic surgery, monitoring orthodontic treatment progress, surgical prediction planning, assessment of surgical change, monitoring skeletal relapse.
Recently CBCT replaced cephalometric analysis for diagnosis, planning, 3D models, or post-surgical evaluation.
Curve of Spee
An increased curve of Spee is also vertical finding that can disguise a significant sagittal discrepancy. A significant curve of Spee correspond with a shortened arch length of the mandible. If a significant curve of Spee were to be leveled, the arch length of the mandible would increase. This is often the case in skeletal class III relationships. Initially, only a minor negative over-jet may exists, but if there is a significant curve of Spee that is then leveled, the negative over-jet can increase dramatically. If this relationship is unnoticed during the initial examination, the original treatment plan may need to be altered dramatically.
There are three main methods for leveling the curve of Spee:
- anterior intrusion
- continuous arch wire/reverse curve Spee (intrusion of anterior teeth, proclination of the anterior teeth, distal tipping of the lower posterior teeth, extrusion of premolars / molars)
- posterior extrusion (upright posterior and anterior teeth/ mesially tipped posterior teeth, upright anterior teeth/ mesially tipped posterior teeth, distally tipped anterior teeth).
Mandible to maxilla relationship
The antero-posterior position of the mandible in relation to the maxilla must be evaluated at the patient who seeks orthognathic surgery.
A functional shift of the mandible to mask the real deformity cannot be detected without a period of muscular deprogramming with an occlusal splint. It takes an experienced and detailed practitioner to ensure true mandibular position is being recorded during a clinical examination.
Lip/Incisor Relationships
One of the most important of these interactions between the skeletal and dental units with the soft tissue is the relationship between the maxillary incisors and the upper lip.
The following measurements should be recorded during the clinical examination of a prospective candidate for orthognathic surgery: upper incisor show at repose and at smile, length of upper lip, sulcus depth.
The keys to proper dento-skeletal planning: upper incisor positioning, AP and vertical position of the maxilla and mandible, central line, occlusal cant, mandibular angle, maxillo-mandibular rotation, overbite/over-jet, vertical dimension, chin position and symmetry, lower facial height, lower lip curvature.
Facial symmetry, evaluated clinicaly and on photographs, is very important in the assessment of the vertical and transversal growth disturbances, most of them with TMJ pathologies (hyperplasia, hypertrophies). We must evaluate: vertical and transversal facial symmetry/lower lip, chin and throat angle/facial convexity/nose, para-nasal area and orbit/sclera show/ears shape and positions.
Temporo-mandibular Joint Function: pain, movements, asymmetries. CBCT registration of the correct position of the condyle into the glenoid fossa is a must in order to reproduce it after mandibular surgery (prevention of condylar sag).
Successful orthognathic surgery cases depend on correct diagnosis and collaboration orthodontist – maxillofacial surgeon in the right order :
- orthodontist - to decompensate the teeth, to prepare the occlusion for the surgery
- maxillofacial surgery
- post-surgical orthodontics to correct the occlusion (posterior open bites, small occlusal discrepancies,etc).
In limited cases, when the deformity is not severe, the surgery is done as first stage, followed by orthodontic treatment.
Orthodontist plays a key role in orthognathic surgery cases, his dedication in diagnosis, pre-surgical and post-surgical treatments, is crucial in achievement good results, in prevention of the complications and relapse.
References
- Blair V P. Operations on the jaw-bone and face. Surg Gynecol Obstet. 1907;4:67–78
- Lübbers H T, Medinger L, Kruse A, Grätz K W, Matthews F. Precision and accuracy of the 3dMD photogrammetric system in craniomaxillofacial application. J Craniofac Surg. 2010;21(3):763–767
- Noar J H, Pabari S. Cone beam computed tomography—current understanding and evidence for its orthodontic applications? J Orthod. 2013;40(1):5–13.
- Sarver D, Jacobson R S. The aesthetic dentofacial analysis. Clin Plast Surg. 2007;34(3):369–394.










 0745 100 497
0745 100 497


